My own questions to the surgeons I consulted with, I had a lot of personal questions based off of my history (like my short teeth roots and how to best save them, the palate expander I had already placed in etc). I don’t think I was able to get through all of these questions, and others were answered as conversation flowed.
Just a note: I feel most at ease, as strange as it sounds, knowing all of the worst case scenarios. So for me personally, I asked about every possible bad thing that I could find or imagine from a TJR + Le Fort + Genioplasty. You do not have to think about all of these questions if you don’t want to! I placed a ” * ” before sections or sentences that I thought might be overly anxious thoughts if that is something you would prefer not to read.
Surgeons I consulted with:
- Surgeons I would have gone with:
- Dr. Sullivan (ended up going with him)
- Dr. Movahed
- Dr. Sanovich
- Surgeons I liked but personally didn’t want to go with based on conversations with other patients of theirs or their treatment plan for me
- Dr. Wolford
- Dr. Shah (recommended not doing TJR and doing SFOT alone)
My Question List to Surgeons:
- What do you think my odds are of success? Do my odds get worse waiting?
- How do we know if I have active ICR and it hasn’t stabilized?
- What about these other surgery options A, B and C that have been recommended to me – do you think there is a good chance of them working? Why or why not?
- What happens if I get the surgery and I am still in pain – isn’t this the end game, nothing more can be done after this surgery? The joints are gone, that is irreversible.
- Do you do metal allergy testing and have you gone through the FDA compassionate use before for the all titanium joints (both FDA and operating hospital has to agree to the documents, it is a longer process and if the surgeon is not as familiar with it it might take more time on your part managing it. Surgery dates have been pushed off for these problems alone. ALWAYS DO METAL ALLERGY TESTING BEFORE GETTING THE JOINTS! Even if the surgeon says it is not needed.)
- *What are chances of developing a metal allergy years from now?
- *If there’s a wear rate, then there’s an accumulation of microparticles – The question now becomes one of whether the particles become antigenic and initiate an inflammatory reaction.
- *Could also cause inflammation, large cell attacks and Antigenic reaction triggering immune response
- *What are chances of developing a metal allergy years from now?
- Is there a possibility of the body rejecting this piece somehow?Even without allergies to metals? I am sensitive when I put in earrings and am afraid.
- *Poor surgical technique and implant design cause implant failure, yet 10–15% of patients experience aseptic implant failure despite well-designed implants and meticulous surgical technique.1
- *“We propose that the release of titanium nanoparticles may contribute to aseptic implant loosening by negatively influencing periprosthetic skeletal repair cells.”1
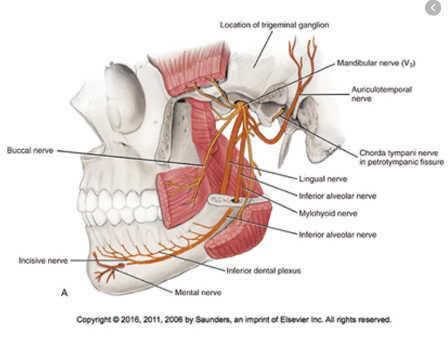
- How possible is nerve damage with this, can you clearly see the nerves and move them out of the way while operating? Resulting in even more permanent pain?
- Do you think I would have any scarring from my first surgery that would bring the blood vessels or nerves closer to my TJR surgical cuts?
- *How often have you experienced vessel hemorrhaging in your surgeries?
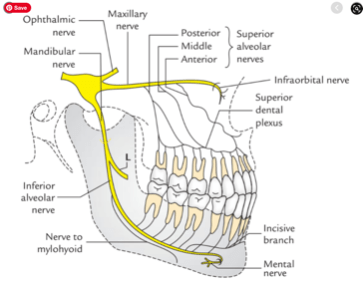
- Can you clearly see the alveolar nerve before placing the screws or is this hidden under bone? (they should say that the scanning software clearly sees the nerves and TMJ concepts plans around the nerves.)
8. Do you know how far out we might be from using future bone rebuilding techniques/ adult stem cells to recreate condyle bones? http://news.bbc.co.uk/2/hi/health/8290138.stm
9. What about a rib graft instead? Would last 40 years, I am still possibly young enough to have
10. What percentage and number of your patients have relapse/ the surgery was not successful for some reason? Have complications?
- How often does revision surgery need to be made for scar tissue buildup limiting function or unwanted bone developing around implants? https://tmjconcepts.com/tmj/files/TMJ-Patient-Information-Brochure_52-0100-G.pdf (there used to be an article on TMJ concepts website about this but it was taken off when Stryker acquired them, unfortunately. I did not save the pdf.)
11. Can the nose collapse after the surgery or a deviated septum appears? (I ended up getting a deviated septum, my maxilla was moved forward 6-7mm)
12. *What are EVERY complication you have seen?
- *Possible complications:
- What if I have active ICR while waiting months for my joint replacements and now the prosthetic joints don’t fit. Or could my teeth not meet up anymore??
- Ear infections so bad the plastic fossa has to be removed
- Droopy eye socket
- Perforated sinuses
- Fibrous non-occlusion (le fort does not fuse)
- TJR components come loose/ screws loosen because they don’t adhere to the bone somehow?
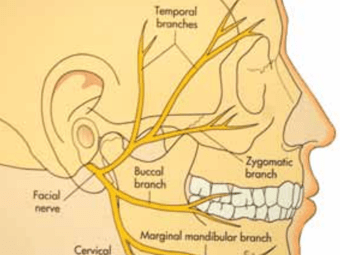
- Not able to move eyebrows or smile normally
- Nose spreads/ getting larger
13. Will I be able to eat steak, chicken, sandwiches, salad and nuts normally again?
14. Do I need surgical braces if I do this? Orthodontic braces next?? Can I do Invisalign pre and post op alone?
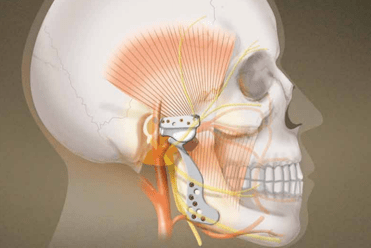
15. How long will the artificial joints (TMJ Concepts, Inc.) last for? I know their company does research that says forever but my previous surgeons and BBC said 15-20 years and it needs to be replaced. That’s at age 45, 60, and 75 at worst for me.
- *Longevity further Q
- How can your body handle that? Unscrewing those areas and then re-screwing in the same areas surely weakens the bone and the TJR components could become loose. Which I hear is a problem.
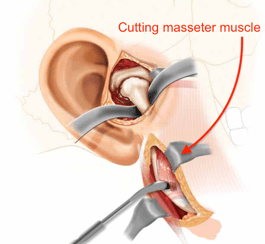
- Cutting through that muscle once more and the scar tissue?
- How many people have you done replacements for and how many years out were they?
16. What exactly is the fossa prothesis made of, what kind of plastic? I thought the body would reject plastic.
17. How do you know exactly where to cut the condyle bone at?
18. Specifically what muscles do you need to cut through during the surgery and what muscles atrophy?
- Cut through the masseter muscles, does this have to be done again and again with every joint replacement?
- Do you get rid totally of the pterygoid muscle? Would I keep this muscle on a rib graft?

20. What do you think of Drs A, B and C that I am working with. Do you think they have produced good work?? (Doctors will almost always try to avoid speaking bad of one another if they have a working relationship. It’s ok to press them a little more for these answers IMO, sometimes you can kind of tell from body language. Ask “If I were your daughter would you send me to her/him?)
21. Are there plates/ screws that need to be removed after the surgery or they are permanent? I have seen people post about “getting these out” after surgery like they are allergic or bothered by them for some reason, maybe because of the cold.
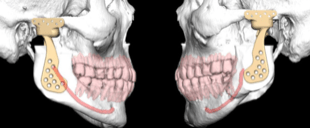
22. Can you do modeling to show me what I will look like after the TJR? Face and airway?
23. Do you do fat grafting to fill the cavity around the prosthesis? Why or why not? (a lot of out of network surgeons use fat grafts based off of Wolford’s research many years ago, helps to prevent excess bone growth)
24. If I have the surgery will you alone perform it and place in the joints or would there be a resident or someone learning in my surgery? I would really prefer there be no one learning in my surgery, I have had bad experiences. (I ended up having residents cut me open and stitch me back but not operate on me directly. I realized Dr. Sullivan really needed them to complete the surgery in record time, I think he only took 4.5-5 hours on my surgery!! I think I had less swelling and nerve damage maybe from this)
25. How frequently will I see you after surgery? 3mos? 6 mos? Annually? Do I get to see YOU directly or will I not be able to and see residents and doctors you are training instead?
26. How many of these surgeries do you do each year, and how many have you done over your career? Who trained you in these surgeries?
27. Do you use custom or stock joints? Tmj concepts? (I prefer the TMJ concepts joints since they are custom made)
28. Am I a pretty straightforward case or a complex case? Could I talk to other patients of yours that looked like me before surgery? Or see their scans?
29. How much does replacement cost if I have to replace these artificial joints later/ what exactly gets replaced….all of it again? Same screw holds? Would hold less well the second time??
30. How do you fight infection and is bony growth a concern at all here? I heard that if the infection gets too bad then the TJ would have to be removed….
- *A 10 year review of TMJ prothesis showed that 4.5% of TJ’s developed infection and all had to be removed despite antibiotic treatment.2
- *Another review said it was 2.5% infection rate. I got an infection after scoliosis surgery and after my MSE insertion personally, I had no infection from my TJR but technically you are always at risk for infection with a biofilm.3
31. Study “Alloplastic reconstruction of the temporomandibular joint” says, “Studies report that up to 88% of TMJR patients experience long term quality of life improvement as a result of decreased pain and increased mandibular function (3, 4, 5)” 2
- What do you think went wrong with the 12% that didn’t do well after TJR? How do I look in regards to this 12%/Can you scout for these people before hand that you think will not benefit from TJR or have poor outcomes?
32. Would I possibly have insufficient quantity or quality of bone to support the TJ components? I have been told I have small bones before. And my mandible seems underdeveloped, says the Piper clinic.
33. Do you use computer aided technology to design the joint and the splint/ virtual surgery planning techniques?
34. What does the recovery look like?
- Considering…
- Time – when do people return back to work
- Very liquid diet
- Nerve pain (read 6 months)
- Inability to move eyebrows up or smile normally
- Braces?
- Sleeping upright?
- PT?
35. Will I need genioplasty?
- Saw that the Mental nerve exits the chin area… risk of damaging this/ how does a genioplasty work with this nerve?
- IS IT BETTER to do genioplasty in a future surgery to prevent nerve damage. Dr. shah said it is better to spread out things into multiple surgeries, less chance of nerve damage this way.
36. Do you recommend any orthodontists in my area/ even out of my area?
37. Tips on insurance- getting them to pay? Who do I talk to about this?
38. Cost estimate for surgery and hospital fees
39. What happens during the surgery if you cut me open and the joint prosthesis does not fit for some reason. How many times has this happened to you and what is the cause of this happening?
40. Is fibrotic scaring a huge concern?
41. In the future if I have a TJR again in my 50s or something, do I have to get braces again?
42. How often do you have to replace implants not due to wear and tear but to the prosthetic loosening it’s grip on the bone?
43. What are all my options towards fixing this?
*Other things I wanted to maybe bring up to surgeons:
1. “A facial asymmetry linked to paresis of the facial nerve (frontal, palpebral, chin), more or less important and more or less long in time depending on the indication of the replacement, the number of operations, the age and the duration of the intervention. Full recovery can take up to 3 years.” 4
2. Causes of failure: “Several events can lead to failure, most of which are theoretical because the failure rate is low”:
- Reasons:
- “Immediate or late postoperative infection (2.5% of patients and less than 2% of operative sites). Immediately, she must ask questions about intraoperative and postoperative hygiene. Late, she said that she brought up the quality of postoperative care and the field (immunosuppression);
- like any prosthesis, a fracture can occur because of constraints either related to the activity or due to long-term trauma;
- prosthetic wear;
- anatomical changes in degenerative disease;
- an allergy to any of the components or a foreign body reaction discovered after implantation.”5
3. Virtual Planning:
“Digital Imaging and Communications in Medicine (DICOM) data allow 3D reconstructions that will serve as a basis for discussion between engineers and surgeons leading to the final position of the mandible and maxillary prostheses.
From the 3D reconstructions, the areas of interest will be identified. These are areas of bone resection (aiming to restore oral dynamics) and bone modeling (aiming to adapt the prosthetic shape as closely as possible to the anatomy)
Virtually, the total prosthetic replacement is carried out taking into account the joint and the potential risks of intramandibular nerve damage associated with the insertion of the screws.” (unsure where this research of mine came from…)
4. The most common complications associated with TMJR (besides those common to all TMJ procedures) include the following:
- Infection,
- A wide range of the face (ears, eyes, hair ,face) has to be disinfected
- Do not hesitate to regularly disinfect the operating sites during the operation
- pain/worsening of TMJ symptoms,
- breakdown and loosening of the prosthesis,
- facial nerve injuries and metal hypersensitivity.
*Maybe Ask right before TJR
- How do plates end up breaking? How do I prevent this from happening?
- Branches of the external carotid artery, namely the superficial temporal and transverse facial, and branches of the internal maxillary artery provide the primary blood supply to the TMJ. The surgeon should be intimately aware of the close proximity of the internal carotid artery and internal jugular vein passing just posteromedial to the medial aspect of the condyle. Devastating hemorrhage may occur from inadvertent injury to these vessels secondary to the limited access for vascular control.
- Heard that if you blow your nose too soon after surgery you can blow nasal mucus through your tear duct?! A DJS patient mentioned this on a forum and 2 people commented that this also happened to them.
- How do I make sure that my metal condyle does not become dislocated ever from the fossa prothesis?
Please feel free to add more comments to the bottom of this post if you asked a question you thought was helpful! Much love to you all and a big virtual hug ❤️
Citations
- “Local Cellular Responses to Titanium Dioxide from Orthopedic Implants” https://www.liebertpub.com/doi/full/10.1089/biores.2017.0017?fbclid=IwAR0WsbJX8gBDcz88npiH3hdzVXV9tYdoKzuE0LdsBuYRaq_iOsK6pbHHovM#B8%20B9%20B10
- “Alloplastic reconstruction of the temporomandibular joint” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5750826/
- “Management of the infected temporomandibular joint total joint prosthesis” https://pubmed.ncbi.nlm.nih.gov/20822842/
- “Facial Nerve Trauma: Evaluation and Considerations in Management” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4329040/ I don’t think this was the exact article, but there is other helpful research on there about facial nerves.
- www-sciencedirect-com.srv-proxy2.library.tamu.edu/science/article/pii/S2213653316300702?via%3Dihub#bib0080


Leave a comment