A little-longish story of how an Ogre became a Bionic Babe 💪 I feel like I recognize myself more in my face as the swelling goes down and I see more pictures my parents have shown me from my childhood. (and by Ogre I mean my last post when I felt huge from all the swelling)
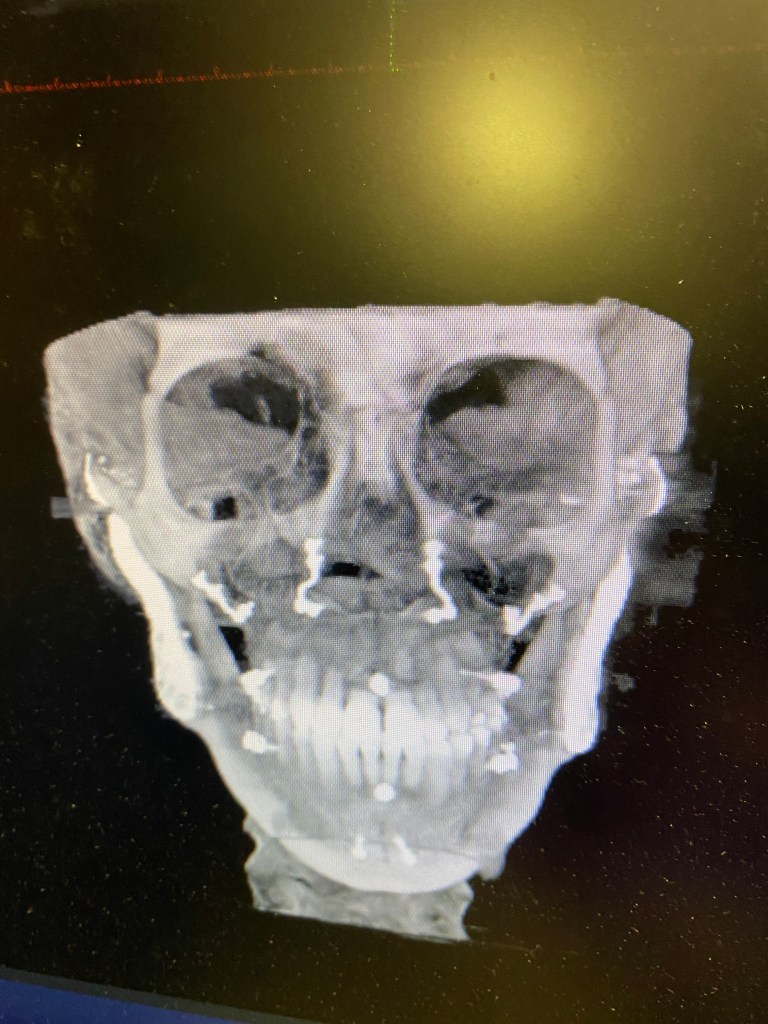
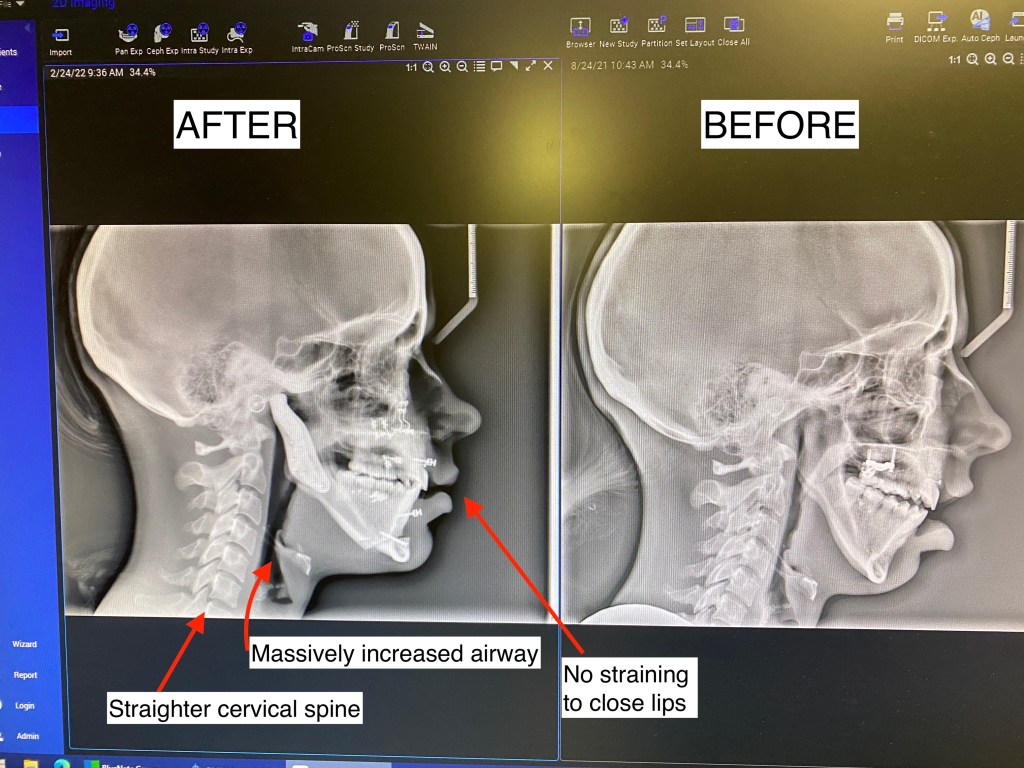
It has been a FULL WEEK since my surgery!! It feels like it has gone by so fast! First off, I want to start this post by showing my first before and after Xray which I couldn’t be happier about!! Look at that airway. I am so thankful now that this surgery was an option for me. I spent a long time rightfully being scared of it, but did the amount of research I felt comfortable with and felt like I knew my own personal pain / TMJ issues well enough going into it to to decide for myself if I thought it would give me a better shot at living. It took me a full year to fully research, consult with 4-5 different jaw surgeons, and talk with anywhere from 100-200 patients online (I’m not even kidding. I am very careful with my health and decisions after what happened to me in the past with jaw treatments and extreme orthodontic work). I was talking with one of my good ICR friends a while back who also researches a lot and we kind of laughed that we envy the people who go into this blind and just get perfect results. No worry or anxiety.
- Airway: Before I had TJR, my airway was 2mm at the narrowest point as
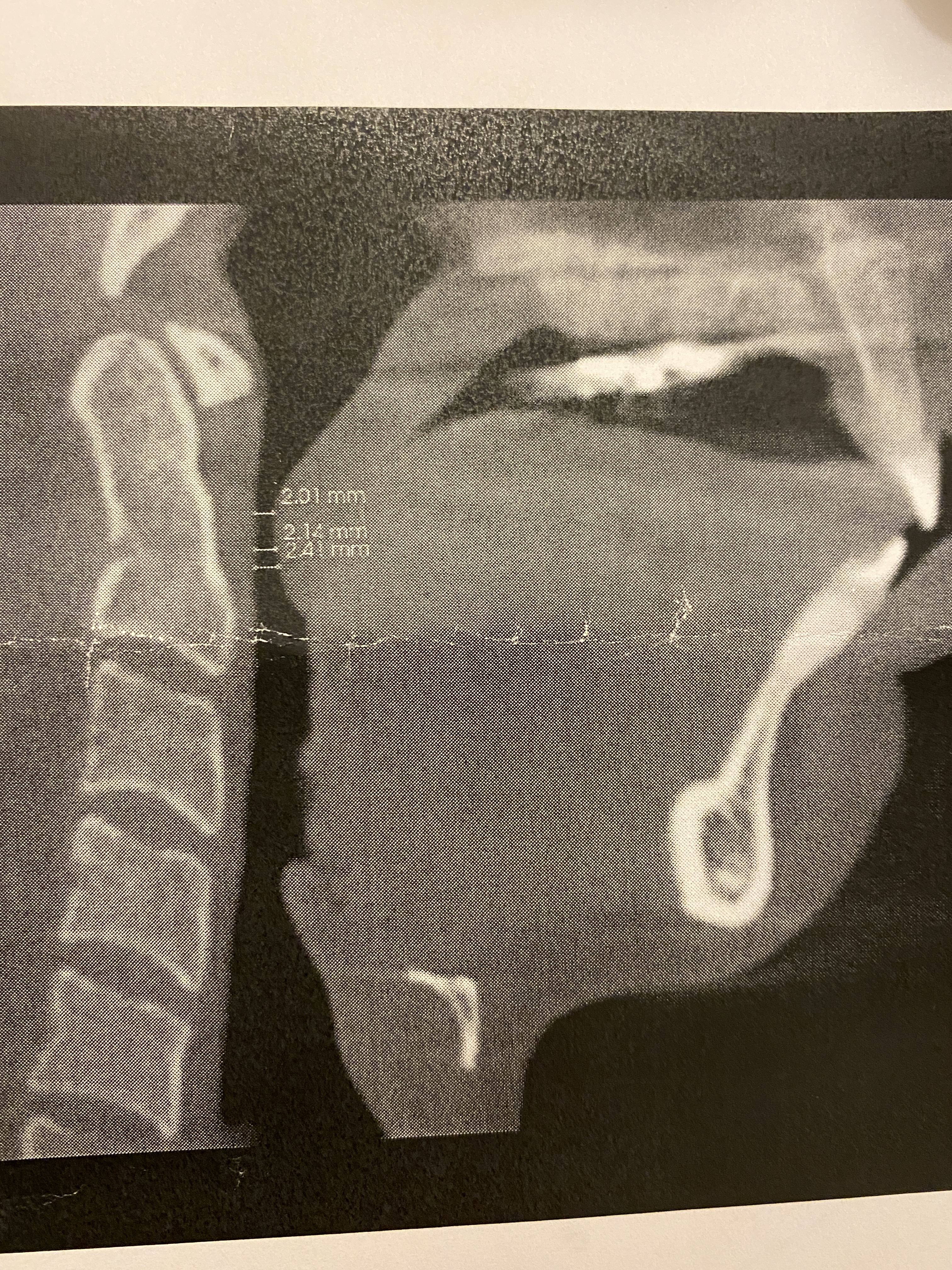 measured by my sleep doctor, which made sense why,
measured by my sleep doctor, which made sense why,- I struggled to swallow pills
- My oxygen levels would drop at night and I was diagnosed with UARS (Upper Airway Resistance Syndrome)
- Received 50% less REM sleep compared to other healthy adults in my sleep test
- 1-3 times a month would wake up choking/gasping (that I could remember), and snored a little. I always slept on my side and never on my back to make breathing easier. I was a stomach sleeper on and off age 12-16, I at one point thought that had caused my TMJ issues 🤷♀️ (could have…). Usually ICR is the perfect storm of many things and not one singular thing.
- I would hyperventilate with extreme cardio exercise ( I thought I was dying one time, literally was on the gym floor sobbing and gasping). I once had a jaw surgeon tell me that “dentists were real ‘hot’ on this airway stuff” but he didn’t seem to think it accounted for much. He also accepted that he just had not studied it enough yet. I think it is all it is made out to be, but time will tell as this year progresses and I can see if any of my fatigue, mental fog and anxiety levels go down with better quality sleep.
- Forward Head Posture/ cervical spine: As the mandible dips back from ICR, it presses on the airway causing the head to tilt forward and the neck to crane in order to open up the soft tissue of the airway enough to receive adequate oxygen. I’m so thankful the body adapts, but these adaptations are not without consequences and many of the consequences we still don’t medically have a good grasp on to know just how far reaching they are to other systems in the body.
- My post op x-ray shows a straighter head posture! I have been seeing a chiropractor the past few years to help manage some of my chronic pain, so I imagine he will be very happy to see this!
- Lips are closed: It is HEALTHY to breathe through the nose and to have your lips closed. Those with ICR are unable to do this without muscle strain, which encourages mouth breathing. Mouth breathing causes all. kinds. of. problems. You can read more about them here if you are interested: https://www.endur.com/blogs/blog/8-scary-consequences-of-mouth-breathing
Update on the last 2 days
The last two days have been pretty good! Days 1-5 of my surgery were the hardest. I hear this is common with other patients as well, I was thinking “Why did I do this”, “When will this end”, “I feel so weird”, “When can I have pain med” etc. I felt dizzy, weak, and like a truck had just impacted my face. At the bottom I will share more details of the last week to anyone considering TJR surgery, just so you know what I personally experienced!
I have been spending the last few days enjoying being wrapped in my heated blanket, hanging over my humidifier, being annoyed at my thumb still in its splint, being loved and supported by my awesome mom and dad (who go 100% out of their way for their 30 yr old adult daughter) and being really doted on by an extremely loving and patient husband.
Rick has pureed my soups, kept a medicine spreadsheet and reminded me of times to take my medicine, crushed my pills, syringe feeds me like a mother bird 😭😭, and is just all around selfless, patient, empathetic to my needs and I just can’t believe he is mine. He had to do all this same stuff for my first jaw surgery while I was in gradschool in 2016, I had chronic pain and TMJ issues already by the time we were dating in college and I don’t know how he keeps it together. I don’t know what I would do with out him in the most literal way I can state this and I hope I am not always in a constant state of sickness / chronic pain for him. I want to get better for him and for myself.





While everything has been going well, I have had two main problems so far:
- Moderate to severe deviated septum that deviated high and far back, due to the anesthesiologist’s poor removal of the endotracheal tube. Dr. Sullivan thinned the bone that the septum sits over (I think common for Le Forts?) then performed a septal suture to keep my nose on the middle plane of my face basically. But that got knocked right out.
- Trouble with swallowing […….continued below]
– Family and friends ❤️- if you want to stop reading here, totally fine. Before you go – feel free to watch the video below, it’s a quick animation from my surgeon on the surgery I had that is very clear. Please pray that my swallowing gets less scary and that my deviated septum can be remediated easily. Thank you guys for your messages and prayers!!
Deviated Septum: I noticed I couldn’t really breathe out of my left nostril and we saw my nose was crooked, but we thought it could just be due to swelling. I honestly couldn’t really breathe anyways because after a Le Fort your sinuses fill with blood. I am still super congested and have had some rough moments feeling like I have been unable to breathe. Just to state: this is pretty rare for Dr. Sullivan to have a deviated septum from these surgeries and was not his fault. I have talked to 2 other ICR patients online that this has also happened to, so maybe not as rare as I thought overall.


On Thursday, Dr. Sullivan met me in his office to see if he could pop the septum back into place. He placed me on an IV with some Versed and numbed my nose but I. Felt. Everything. I was also very anxious going into it and had not had any pain medication since 12:00am the night before. He pushed and pushed, and then placed in some packing into my nose with iodine and some other sort of medication to help clear my painful left sinus, and then stitched the packing to my nose so I didn’t inhale it / it stayed put. This was in an effort to keep the septum in place. I think my septum has continued to deviate however, and my congestion, sinus pressure, and hearing have gotten worse. So one of his residents is just going to remove it tomorrow. We have some options for what to do, possibly re-operating which I am not excited about obviously. But let’s pray that my septum pops over tomorrow somehow! 😬 The packing has been painful so I’m ready to have it taken out.
Swallowing: Oh my goodness. So when I first woke up out of anesthesia I noticed my tongue was on a completely different part of my palate. I could now expand my tongue outwards to be uncramped, but it took this full week to break that muscle memory. Even as I sit here my tongue is maybe 1/2 cm not seated correctly. During my undergrad years 2010-2014 my TMJ physical therapist taught me proper tongue and resting posture to help my pain, which really did help me a lot back then even within the constraints we were working with. So, back to swallowing. When I swallow right now, I either:
- Swallow a lot of Air
- Swallow liquids UP my nose somehow instead of down
- Or it rebounds out of my throat and comes jetting out of my mouth
It’s better if I am thinking when I am swallowing, if I’m distracted and not paying attention when I swallow it’s def gonna be a bad swallow with my old pattern. Like when I reached for a glass of water first thing this morning and did my thing and then 1/2 water went down my throat and the other half dribbled out. This is not because I am numb, I can feel my top lip 95% now and my bottom lip 85% now. Palate is still 60% numb however, L of tongue is 5% numb…just enough to annoy me :).
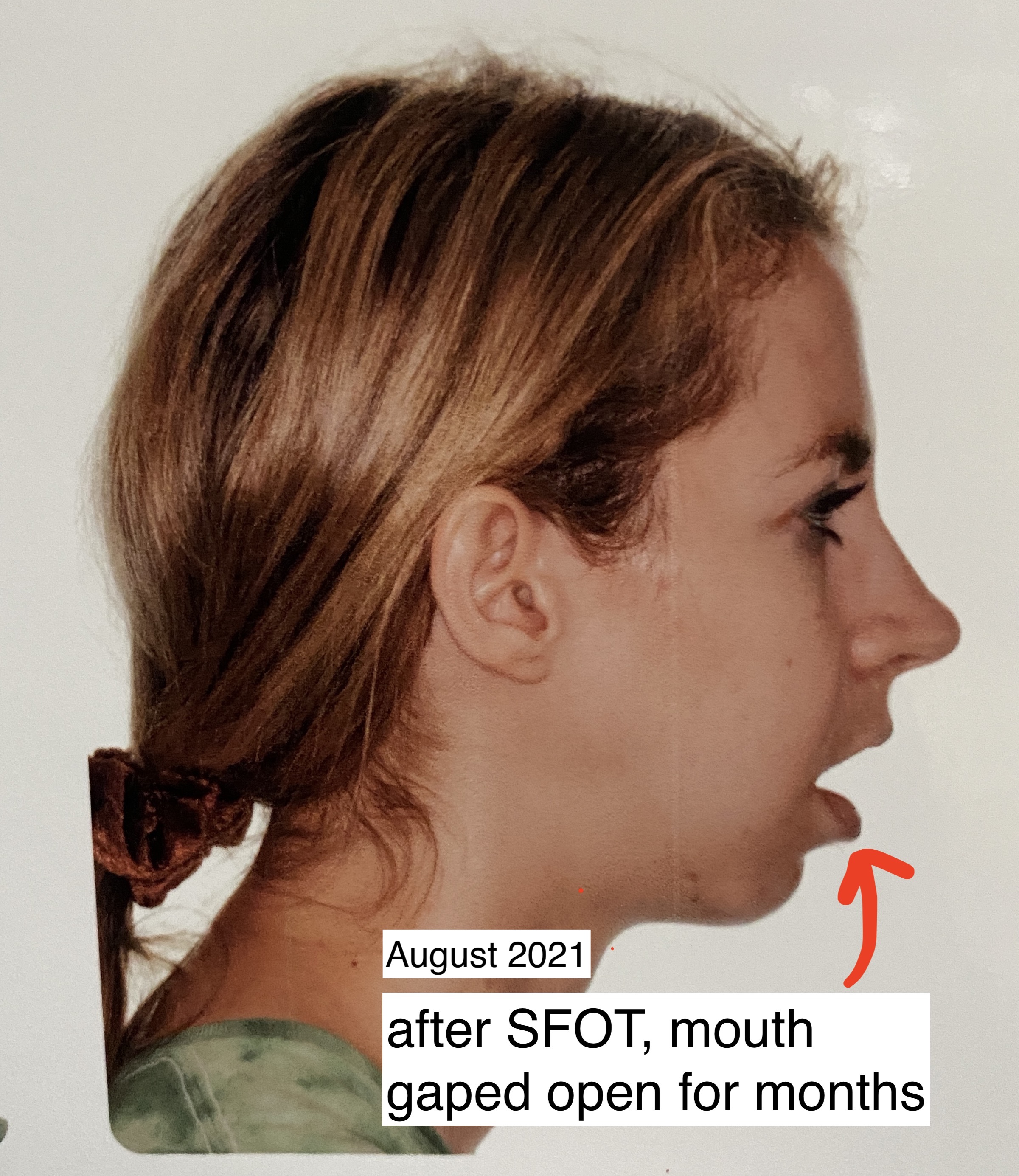
I hope this gets better, and I imagine my soft tissue is needing to settle around for a little bit as well. My soft tissue had another change May 2021 from my SFOT surgery and my lips had to have a few months to settle in with the new bite, I imagine the back of my throat could be the same?

For those considering TJR (or just want to keep reading),
I will go into just a little further detail about this week and give a short vlog of my talking progress:
- Days 1-3 in Hospital
- 3rd day most painful: I wanted to stay in the hospital at least 3 nights. I heard the 3rd day was the most painful and I wanted to be on IV morphine + toradol for that. They tried to get me to leave after the first day, but my family and surgical team went to bat for me❤️
- Some people get sick. It is ok if you need to expel. The banding will protect you. You will also receive IV antinausea medicine, let your anesthesiologist know if you have a prior history of getting nauseous on anesthesia. I requested some IV nausea med when I had to take ground up ibuprofen, that one is by far the worst taste. Maybe you can come with liquid kids ibuprofen and the nurses could give you the same dose?
- IV Antibiotics: I also wanted to be on IV antibiotic for 3 days at least. When I consulted with Dr. Wolford, he said that he used 2 different IV antibiotics on patients for 5 or so days in the hospital, and he had a very low infection rate (it had been 2-3 years since his last infection when I talked with him Jan 2021.) There is a LOT more to infections, you really are never out of the clear to get a TJR infection even years out, but this was just my personal preference. I noticed at Mercy Hospital they alternated 2 types of IV antibiotics on me as well. Infections were one of the scarier parts of this surgery for me, with rates averaging between 1-4.5%1,2 depending on what articles you read. And it more often than not requires a second surgery and prosthesis removal to remedy. Each time you are opened up for jaw surgeries, your prognosis could get worse as scar tissue brings your nerves and arteries closer together and harder to find.
- Days 3-5
- My swelling was at its peak, and the first night home from the hospital was the hardest. I was on,
- Augmentin (3xs per day, crushed and mixed with chocolate syrup bc this stuff nasty)
- Ibuprofen (every 6 hrs)
- Norco (every 6 hrs, alternating with Ibuprofen)
- Chlorhexidinegluconate mouthwash to clean my Le fort / Genio incisions and TADS (2xs per day)
- Methylprednisolone (steroid for swelling, started 5th day)
- Ondansetron (nausea med, needed only 2)
- Small amounts of Klonopin and Trazodone as needed for clenching (I had a personal prescription for this from my PCP and highly recommend if you are a clencher. This has helped my muscles not hurt so much from being stretched in all different ways post TJR, helped my post op anxiety and also my ability to sleep better! Have to be VERY careful to take them as far apart from the norco as possible, I believe I did have some slowed breathing at points and backed off these meds some. I’m even worried posting this, I’m not a doctor so please talk with your doc about this, this is just what has helped me a lot)
- Sudafed and saline nasal spray
- My swelling was at its peak, and the first night home from the hospital was the hardest. I was on,
- Days 6-7
- Still taking all the same medication above, but not waking up anymore to take pain med at night.
- The mornings and afternoon are good, but generally towards the end of the day my “joints” start to hurt and that’s when it’s time to go to bed
- I feel happy. Just want to put this in here❤️
1 week post op | Swelling and Feeling :
- Swelling
- Face near joints and under eyes and cheeks are still swollen and puffy but going down, most swollen part is around the genio area
- I have yellow bruising that has slowly appeared down my neck the last few days. My ICR friend told me this is another sign that your body is modifying your swelling and inflammation at this point.

- Feeling– in % of what I can feel (ex: 95% have the feeling back in my lips) – also this is suuuuper arbitrary and everyone’s anatomy and surgical cuts are different. I’ve heard feeling comes back even years later sometimes,
- Top lip 95%
- Bottom lip 85%
- Palate 60%
- L of tongue 95%
- Below eyes 50%
- Cheeks 60%
- Skin over joints 15%
- Chin 5%, I will be asking my surgeon about this one I really can’t feel anything there, not surprising given some things ICR patients told me about this piece of the surgery.
Finally – It is interesting comparing this with my bilateral fat graft diskectomy surgery in 2016, which had a lot more medications and restrictions. If you asked me which surgical experience I prefer, it’s actually TJR I think…even though the first 5 days were understandably miserable. It feels like I am getting better every day and not in the complete mental fog that I was in during the medicated healing process of the fat graft. I feel closer to obtaining function in the next few weeks and months, whereas with the fat graft diskectomy I was restricted in a splint, heavy rubber-banding and surgical braces for 6 months with more and more time in and out of the splint, and was expected to take larger amounts of klonopin and trazodone to relax the muscles enough for the fat graft to become fibrous over those months time. And all that would have been worth it had it worked for me. I have never been able to completely quit taking those medications for the past 5 years due to muscular pain. It really did help my joint pain a TON though.
And to caveat on healing times – I do think I am healing quicker than what is normal for TJR in all fairness, I hope I have not spoken too soon 😬.
And that is my story of how in 7 days I became a ✨bionic babe✨
Citations:
- McKenzie, W. S. (n.d.). Complications following temporomandibular joint replacement: A 10-year retrospective review. aaoms.confex.com. Retrieved February 26, 2022, from https://aaoms.confex.com/aaoms/am1509/webprogram/Paper10871.html
- LG;, M. (n.d.). Avoiding and managing temporomandibular joint total joint replacement surgical site infections. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. Retrieved February 26, 2022, from https://pubmed.ncbi.nlm.nih.gov/22883323/#:~:text=The%20infection%20incidence%20within%202,2%20weeks%20to%2012%20years.

3 responses to “9 | Bionic Babe”
Good job!
So great to watch your progress.
Omg but still scares me to death !
You are a brave one!
LikeLike
Wow. I didn’t know all of this was even possible. I hope you feel like a whole new (bionic) woman and can start enjoying life! ❤️
LikeLike
You’re looking great and you sound like you’re doing great. So happy for you. Thank you for posting your whole journey. It’s very helpful for those still at beginning stages.
LikeLiked by 1 person